Why are Dental Implants so Expensive: Exploring the Cost Factors

“Why are dental implants so expensive?” It’s a question that many individuals contemplating tooth replacement may find themselves asking. The cost of dental implants can indeed be significant, but understanding why can shed light on the value they offer. In this informative guide, we delve into the various factors that contribute to the pricing of […]
Dental Implants Procedure: Everything You Need to Know
Welcome to our comprehensive guide on dental implants procedures! Whether you’re considering dental implants to restore your smile, improve your oral health, or enhance your confidence, we’re here to provide you with all the essential information you need. From understanding the process and benefits to exploring potential risks and alternatives, this blog aims to be […]
Understanding the Process of Dental Implants: How Are Dental Implants Done?
Welcome to our comprehensive guide on the process of dental implants. Whether you’re considering this procedure or simply curious about how it’s done, we’re here to provide you with all the essential information. Dental implants offer a permanent solution for missing teeth, restoring both function and aesthetics to your smile. In this blog, we’ll walk […]
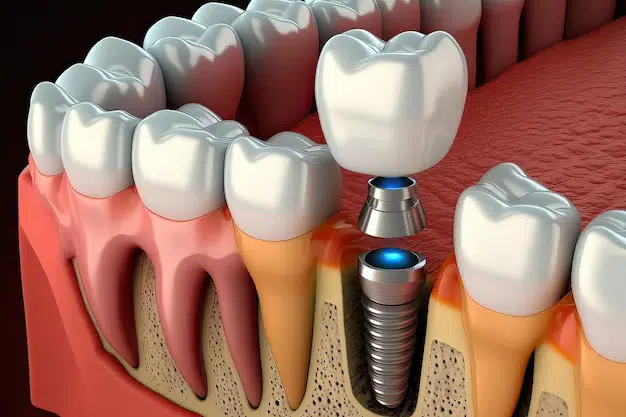
Understanding How Dental Implants Work: A Comprehensive Guide

Welcome to our comprehensive guide on dental implants, where we delve into the intricate details of how Dental Implants work. replacements work. Dental implants have revolutionized the field of dentistry, offering a reliable and long-lasting solution for those missing one or more teeth. In this guide, we’ll explore the anatomy of dental implants, the process […]
How Much Do Dental Implants Cost? Investing for Change
Dental Implants have arisen as a noteworthy answer for people wrestling with tooth misfortune, offering an extremely durable and regular-looking option in contrast to scaffolds or false teeth. While the advantages of dental implants are obvious, one pivotal perspective frequently remains in the front direction – the expense. In this blog entry, we dig into […]
How to Get Free Dental Implants UK? Achieving Financially Fit Smiles

Dental inserts assume a vital part in reestablishing oral well-being and certainty, giving an extremely durable answer for missing teeth. In any case, the significant expense related to dental embed systems represents a huge boundary for some people. In this blog, we will dig into the significance of dental embeds, and their effect on general […]
Do Dental Implants Hurt? Understanding Discomfort

Dental implants have revolutionized modern dentistry, offering a lasting solution for tooth replacement. However, the concern surrounding pain remains a significant factor that can influence individuals’ decisions. This comprehensive guide aims to address these concerns by providing an in-depth exploration of do dental implants hurt. Brief Overview of Dental Implants Dental implants are […]
How Long Do Dental Implants Last? The Answer May Surprise You!

One of the most common questions surrounding dental implants is, “How long do dental implants last?” The answer to this question is multifaceted, and understanding the factors that contribute to the longevity of dental implants can help individuals make informed decisions about their oral health. Dental implants have revolutionized the field of dentistry, offering a […]
Are Dental Implants Permanent: Your Smile is Our Top Priority

Introduction Your smile is a powerful asset, influencing not only your appearance but also your confidence and overall well-being. Are Dental Implants Permanent? For individuals grappling with tooth loss, dental implants have emerged as a revolutionary solution, providing a natural-looking and functional alternative. The question on many minds, however, is whether dental implants are […]
