“Why are dental implants so expensive?” It’s a question that many individuals contemplating tooth replacement may find themselves asking. The cost of dental implants can indeed be significant, but understanding why can shed light on the value they offer. In this informative guide, we delve into the various factors that contribute to the pricing of dental implants. From materials and expertise to geographic location and alternatives, we aim to demystify the economics behind this essential dental procedure.
Why Are Dental Implants So Expensive?
Dental implants often come with a hefty price tag, leaving many wondering why they’re so costly. Several factors contribute to their expense. Dental implants are made from high-quality materials such as titanium, which is biocompatible and durable, ensuring long-term success. The expertise required to perform implant surgery is extensive. Pre-operative procedures, such as diagnostic tests and imaging, are essential for assessing the patient’s oral health and planning the implant placement. During the implant placement procedure, patients may require anesthesia or sedation to ensure comfort and relaxation. The use of these medications adds to the total cost of the treatment.
Customization is another factor that influences the cost of dental implants. Geographic location also plays a role in determining the cost of dental implants.Insurance coverage for dental implants is often limited, leaving patients to bear the majority of the cost out of pocket. For those seeking alternatives to traditional implants, options such as dentures or dental bridges may offer a more cost-effective solution.
Importance of Understanding the Factors
Understanding the factors that contribute to the cost of dental implants is crucial for patients considering this treatment option. By gaining insight into why implants are expensive, individuals can make informed decisions about their oral health and finances. One of the primary reasons for understanding the factors influencing implant costs is to manage expectations. Dental implant treatment is a significant investment, both in terms of finances and time. By knowing what contributes to the overall expense, patients can better prepare themselves for the financial commitment involved.
Material Costs
Material costs significantly contribute to why dental implants are so expensive, reflecting the quality and durability of the components used.
Breakdown of Materials Used in Dental Implants
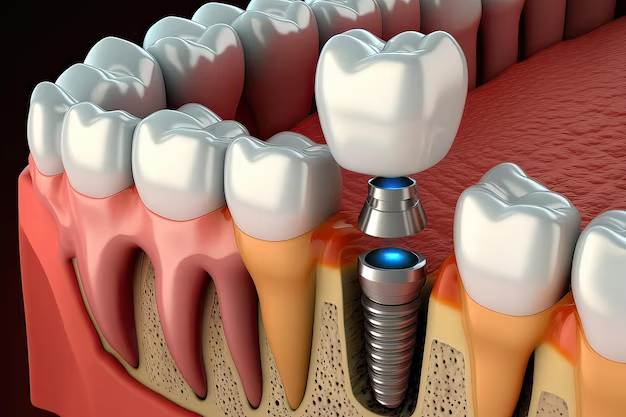
Dental implants are typically made from high-grade materials such as titanium, which is biocompatible and able to integrate seamlessly with the jawbone. Titanium implants are known for their exceptional strength and durability, ensuring long-term stability and functionality.The implant itself consists of several components, including the implant fixture, abutment, and prosthetic tooth or crown. Each of these components must meet stringent quality standards to ensure the success and longevity of the implant.
In addition to titanium, other materials may be used in the construction of dental implants, such as ceramic or zirconia for the prosthetic tooth. These materials are chosen for their natural appearance and ability to withstand the forces of chewing and biting.

Quality and Durability Considerations
The quality and durability of materials used in dental implants directly impact their long-term success and effectiveness. High-quality materials are essential for ensuring the stability and functionality of the implant over time. Titanium implants are preferred for their biocompatibility and ability to fuse with the surrounding bone through a process called osseointegration. This fusion provides a strong foundation for the prosthetic tooth and helps prevent implant failure.
The durability of dental implant materials is crucial for withstanding the forces of daily chewing and biting. High-quality materials can withstand these forces without experiencing wear or damage, ensuring the longevity of the implant.
Impact on Overall Cost
The use of high-quality materials in dental implants contributes to their overall cost, reflecting the investment in materials that provide long-term stability and functionality. While the upfront cost of dental implants may be higher than alternative tooth replacement options, their durability and longevity often result in cost savings over time. Dental implants can last for decades with proper care, making them a worthwhile investment for many patients.
Labor and Expertise
The labor and expertise involved in dental implant procedures contribute significantly to why are dental implants so expensive.
Skill and Training Required
Performing dental implant surgery requires extensive skill and training due to the complexity of the procedure. Dentists, periodontists, and oral surgeons undergo years of education and hands-on experience to master the techniques involved in implant placement.
Implant surgery involves precise placement of the implant fixture into the jawbone, ensuring proper alignment and stability. Additionally, the dentist or surgeon must consider factors such as bone density and gum tissue health to achieve successful outcomes.
Role of Specialists
Specialists such as periodontists and oral surgeons play a crucial role in the success of dental implant procedures. These highly trained professionals have specialized knowledge and experience in implant dentistry, allowing them to provide optimal care for patients undergoing implant treatment.
Periodontists specialize in the treatment of gum disease and the placement of dental implants. Their expertise in periodontal health ensures that the surrounding gum tissue is healthy and able to support the implant. Oral surgeons are trained in surgical procedures involving the mouth, jaws, and facial structures. They possess the skills and knowledge necessary to perform complex implant surgeries, including bone grafting and sinus lifts when additional bone support is needed.
Influence on Pricing
The labor and expertise required for dental implant procedures directly influence their pricing. Specialists such as periodontists and oral surgeons command higher fees due to their advanced training and skill level. In addition to the surgeon’s fees, other factors such as facility fees, anesthesia costs, and pre-operative diagnostics contribute to the overall expense of implant treatment. Patients should consider these factors when budgeting for dental implant surgery.
While the cost of dental implants may initially seem high, the expertise and skill of the dental team are essential for ensuring successful outcomes. Investing in quality care from experienced professionals can lead to long-term benefits and a higher likelihood of implant success.
Pre-operative Procedures
Pre-operative procedures before dental implant surgery contribute to why are dental implants so expensive.
Diagnostic Tests and Imaging
Before undergoing dental implant surgery, patients typically undergo various diagnostic tests and imaging procedures. These tests are essential for assessing the patient’s oral health, identifying any underlying issues, and planning the implant placement accurately.
Common diagnostic tests include dental x-rays, panoramic radiographs, and 3D cone beam computed tomography (CBCT) scans. These imaging techniques provide detailed images of the patient’s teeth, jaws, and surrounding structures, allowing the dental team to evaluate bone density, sinus anatomy, and nerve placement.

Bone Grafting or Sinus Lifts If Necessary
In some cases, patients may require additional procedures such as bone grafting or sinus lifts to prepare the jawbone for dental implant placement. These procedures are necessary when the existing bone structure is insufficient to support the implants adequately. Bone grafting involves transplanting bone tissue from another part of the body or using synthetic materials to augment the jawbone. This procedure helps rebuild lost bone volume and density, providing a stable foundation for the implants.
Similarly, a sinus lift, also known as a sinus augmentation, involves lifting the sinus membrane to create space for bone grafting in the upper jaw. This procedure is necessary when the natural bone height in the posterior maxilla is inadequate for implant placement. Both bone grafting and sinus lifts require additional surgical procedures, materials, and expertise, which contribute to the overall cost of dental implant treatment.
Additional Costs Associated with Preparatory Steps
In addition to diagnostic tests and supplemental procedures, there may be other preparatory steps involved in dental implant treatment that incur additional costs. For example, patients may require extractions of damaged or decayed teeth before implant placement. The extraction process involves anesthesia, surgical tools, and post-operative care, all of which contribute to the overall expense.
Implant Placement Procedure
The complexity and intricacy of the implant placement procedure contribute to why are dental implants so expensive.
Surgical Process and Equipment Used
The surgical process of dental implant placement involves precise techniques and specialized equipment to ensure the accurate placement of the implant fixture into the jawbone. During the procedure, the dentist or oral surgeon makes an incision in the gum tissue to expose the underlying jawbone. Then, using drills and other instruments, they create a small pilot hole in the bone for the implant fixture. Once the pilot hole is prepared, the implant fixture, typically made of biocompatible titanium, is carefully inserted into the jawbone. The dentist ensures proper alignment and depth to achieve optimal stability and integration with the surrounding bone tissue.
Throughout the surgical process, the dental team relies on advanced equipment such as dental drills, implant drivers, and surgical guides to facilitate precise placement and ensure the success of the procedure. The use of specialized surgical equipment and instruments adds to the overall cost of dental implant treatment, reflecting the investment in technology and resources required to achieve successful outcomes.
Anesthesia and Sedation Options
Anesthesia and sedation options are essential for ensuring patient comfort and relaxation during the dental implant placement procedure. Depending on the complexity of the surgery and the patient’s preferences, various anesthesia and sedation options may be available. Local anesthesia is commonly used to numb the surgical area and minimize discomfort during the procedure.
For patients who experience anxiety or fear of dental procedures, sedation options such as oral sedatives, intravenous (IV) sedation, or general anesthesia may be recommended. These medications induce a state of relaxation or unconsciousness, allowing the patient to undergo the procedure comfortably.
Post-operative Care and Monitoring
Following the implant placement procedure, patients require post-operative care and monitoring to ensure proper healing and integration of the implants. The dental team provides instructions for post-operative care, including guidelines for oral hygiene, dietary restrictions, and activity limitations. Patients may also receive prescriptions for pain medication or antibiotics to manage discomfort and prevent infection.
Regular follow-up appointments are scheduled to monitor the healing process and assess the stability of the implants. During these appointments, the dentist or oral surgeon evaluates the condition of the surgical site, checks for signs of infection or complications, and makes any necessary adjustments to the treatment plan.
Customization and Aesthetics
Customization and aesthetics significantly contribute to why are dental implants so expensive, reflecting the meticulous design and fabrication process involved.
Design and Fabrication of Prosthetic Teeth
The design and fabrication of prosthetic teeth for dental implants require precise measurements and high-quality materials to achieve natural-looking and functional results. Dental technicians use advanced techniques such as computer-aided design (CAD) and computer-aided manufacturing (CAM) to create custom prosthetic teeth that match the shape, size, and color of the patient’s natural teeth. These digital technologies allow for precise customization and ensure a seamless integration with the patient’s smile.
High-quality materials such as porcelain or zirconia are commonly used to fabricate prosthetic teeth due to their durability, aesthetics, and biocompatibility. These materials are carefully selected to provide the most natural appearance and optimal function for the patient. The design and fabrication process of prosthetic teeth involves multiple steps, including impressions of the patient’s mouth, digital modeling of the teeth, and milling or shaping of the prosthetic material. Each step requires specialized equipment and expertise, contributing to the overall cost of dental implant treatment.
Matching Implants to Natural Teeth
Matching dental implants to the patient’s natural teeth is essential for achieving a harmonious and seamless smile. Implants must blend seamlessly with the surrounding teeth in terms of color, shape, and alignment to create a natural-looking result. Dental implant crowns or prosthetic teeth are customized to match the color and shade of the patient’s natural teeth, ensuring a cohesive appearance across the entire smile. Additionally, the shape and size of the prosthetic teeth are carefully tailored to complement the patient’s facial features and smile aesthetics.

Impact on Overall Appearance and Function
The customization and aesthetics of dental implants play a significant role in enhancing the overall appearance and function of the patient’s smile. By closely matching the color, shape, and alignment of the prosthetic teeth to the natural dentition, dental implants create a seamless and natural-looking smile. Patients can smile, speak, and chew with confidence, knowing that their dental implants blend harmoniously with their natural teeth. Dental implants provide stability and support for adjacent teeth, preventing shifting or misalignment over time. This helps maintain the integrity of the bite and jaw function, contributing to overall oral health and well-being.
Geographic Location
The cost of dental implant treatment varies significantly depending on the region or country where it is performed. Urban areas and regions with higher living costs generally have higher prices for dental services, including implant treatment. Factors such as rent, labor costs, and overhead expenses contribute to the overall cost of dental care in a particular location.
Patients should consider the geographic location when budgeting for dental implant treatment and explore options for care in different areas to find the most cost-effective solution. While traveling for dental care may incur additional expenses, it could ultimately result in significant cost savings for patients seeking affordable dental implant treatment.
Additional Factors Affecting Cost
One significant factor is facility fees, which cover the overhead costs associated with operating a dental practice or surgical center. These fees may include expenses such as rent, utilities, equipment maintenance, and administrative costs. High-quality facilities with state-of-the-art equipment and amenities may command higher fees, contributing to the overall cost of dental implant treatment.
Insurance coverage also plays a role in determining the out-of-pocket costs for dental implant treatment. While some dental insurance plans offer coverage for implant procedures, coverage levels and limitations vary widely. Many plans consider dental implants to be elective procedures and provide limited or no coverage, leaving patients responsible for the full cost of treatment.
Alternatives to Traditional Implants
Exploring alternatives to traditional dental implants can provide cost-effective options for patients seeking tooth replacement solutions.
While dental implants offer numerous benefits, including durability, stability, and aesthetics, they may not be feasible for everyone due to financial constraints or other factors. Fortunately, several alternative tooth replacement options are available that offer similar benefits at a lower cost.
Dentures are a popular and affordable option for replacing multiple missing teeth or full arches of teeth. Modern dentures are designed to look natural and fit comfortably, providing a functional and aesthetically pleasing solution for patients with missing teeth.
Dental bridges offer another alternative to dental implants for replacing one or more missing teeth. Bridges consist of artificial teeth attached to adjacent natural teeth or dental implants, providing a fixed and permanent solution for tooth replacement.
Conclusion
The high cost of dental implants is influenced by various factors, including material costs, labor and expertise, pre-operative procedures, customization, and geographic location. While the expense of dental implants may seem daunting, it’s important to consider the long-term benefits they offer, such as durability, aesthetics, and improved oral health. Patients should work closely with their dental providers to explore financing options, insurance coverage, and alternative treatments to make informed decisions about their oral health and finances.
FAQs
Are there any financing options available for dental implant treatment?
Yes, many dental practices offer financing options such as payment plans or healthcare financing programs to help patients manage the cost of dental implant treatment.
Does dental insurance cover the cost of dental implants?
Dental insurance coverage for dental implants varies widely depending on the insurance plan. While some plans may offer partial coverage for implant procedures, many consider them to be elective and provide limited or no coverage.
How long do dental implants last?
With proper care and maintenance, dental implants can last for decades or even a lifetime. Regular dental check-ups, good oral hygiene, and avoiding habits like smoking can help prolong the lifespan of dental implants.