Welcome to our comprehensive guide on the process of dental implants. Whether you’re considering this procedure or simply curious about how it’s done, we’re here to provide you with all the essential information. Dental implants offer a permanent solution for missing teeth, restoring both function and aesthetics to your smile. In this blog, we’ll walk you through each step of the implant process, from the initial consultation to the final placement of the restoration.
What are Dental Implants
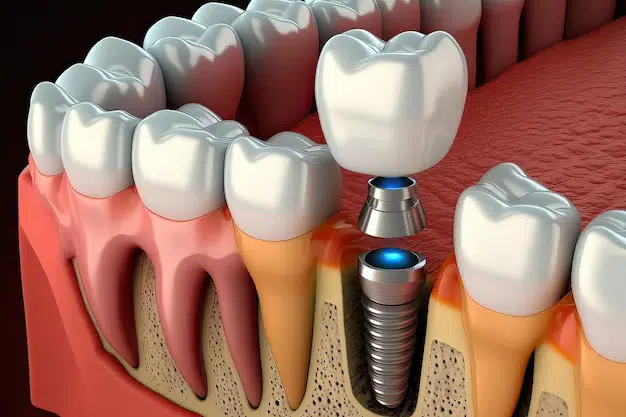
Dental implants are prosthetic tooth roots made of titanium that are surgically placed into the jawbone beneath the gum line. These implants provide a strong foundation for artificial teeth or dental crowns. They are designed to fuse with the natural bone over time through a process called osseointegration, creating a stable and durable anchor for replacement teeth.
Dental implants mimic the function and appearance of natural teeth, offering a long-term solution for individuals with missing teeth or tooth loss due to injury, decay, or disease. By understanding the basics of dental implants, patients can make informed decisions about their oral health and treatment options.
Importance of Understanding the Process of Dental Implants
Understanding the process of dental implants is crucial for anyone considering this treatment option. It involves a series of steps that begin with a comprehensive evaluation and treatment planning by a qualified dental professional. Patients need to have a clear understanding of what to expect before, during, and after the procedure, including potential risks and benefits. Knowing the intricacies of the implant process allows patients to ask informed questions, communicate effectively with their dental team, and make informed decisions about their treatment.
Initial Consultation
Importance of the Initial Consultation
The initial consultation is a crucial step in the dental implant process as it provides an opportunity for both the patient and the dental team to discuss various aspects of the treatment. During this consultation, the dentist or oral surgeon evaluates the patient’s oral health status, including the condition of their remaining teeth, gum health, and jawbone density. Understanding the patient’s oral health history, concerns, and goals allows the dental professional to tailor the treatment plan to meet their specific needs and expectations.
The initial consultation is an opportunity for the patient to ask questions, express any fears or apprehensions they may have, and gain a better understanding of the dental implant procedure. This open communication between the patient and the dental team lays the foundation for a successful treatment outcome.
Patient’s Oral Health History, Concerns, and Goals
During the initial consultation, the dental team gathers essential information about the patient’s oral health history, including any previous dental treatments, existing dental conditions, and medical history. Understanding the patient’s oral health background helps the dentist identify any potential risk factors or contraindications that may impact the success of the dental implant procedure.
The consultation allows the patient to express their concerns, preferences, and goals regarding their oral health and the outcome of the treatment. By actively involving the patient in the decision-making process, the dental team can develop a personalized treatment plan that aligns with the patient’s expectations and priorities. This collaborative approach ensures that the patient feels empowered and informed throughout their dental implant journey.
Examination and Assessment of Jawbone Density and Oral Tissues
Another critical aspect of the initial consultation is the examination and assessment of the patient’s jawbone density and oral tissues. Adequate jawbone volume and density are essential for the successful placement and long-term stability of dental implants. During the consultation, the dentist may perform various diagnostic tests, such as X-rays or CT scans, to evaluate the quality and quantity of the jawbone.
The dentist assesses the condition of the surrounding oral tissues, including the gums and adjacent teeth, to determine if any additional treatments, such as bone grafting or gum disease therapy, are necessary before proceeding with dental implant surgery. This comprehensive evaluation helps the dental team develop a treatment plan that addresses any underlying issues and ensures optimal outcomes for the patient’s dental implant procedure.
Treatment Planning
Treatment Options Based on the Patient’s Needs
During the treatment planning phase of dental implant treatment, the dental team considers various factors to determine the most suitable treatment options for the patient. These factors may include the number of missing teeth, the condition of the remaining teeth and oral tissues, the patient’s oral health history, and their aesthetic preferences.
Based on these considerations, the dentist presents different treatment options to the patient, such as single-tooth implants, implant-supported bridges, or implant-supported dentures. Each option is carefully explained, highlighting its benefits, potential risks, and expected outcomes. The goal is to empower the patient to make an informed decision about their treatment based on their individual needs and preferences.
Digital Imaging to Plan Implant Placement
Digital imaging technology plays a crucial role in the treatment planning process for dental implants. Advanced imaging techniques, such as cone beam computed tomography (CBCT) scans, provide detailed 3D images of the patient’s oral anatomy, including the jawbone, teeth, and surrounding structures. These images allow the dentist to assess the quantity and quality of the jawbone, identify the location of vital structures such as nerves and sinuses, and accurately plan the placement of dental implants.
By visualizing the patient’s oral anatomy in three dimensions, the dental team can develop a precise surgical guide for implant placement, ensuring optimal positioning and stability of the implants. This digital approach enhances the predictability and success of the dental implant procedure while minimizing the risk of complications.
Customized Treatment Plan
Every patient’s dental implant treatment plan is customized to address their unique needs, goals, and oral health status. The treatment plan is developed collaboratively between the patient and the dental team, taking into account factors such as the number and location of missing teeth, the condition of the jawbone, and any existing dental issues. The dentist carefully considers the patient’s long-term oral health and functional requirements when designing the treatment plan, aiming to restore their smile, bite, and overall oral function effectively.
Dental Implant Surgery
Surgical Procedure for Implant Placement
Dental implant surgery is a multi-step procedure aimed at replacing missing teeth with artificial tooth roots made of titanium. The surgery typically involves several key steps, beginning with the preparation of the surgical site and concluding with the placement of the implant posts into the jawbone.
Administration of Local Anesthesia
Before initiating the surgical procedure, the dentist administers local anesthesia to ensure the patient’s comfort throughout the surgery. Local anesthesia numbs the surgical site, preventing the patient from experiencing any pain or discomfort during the procedure. The dentist may also offer sedation options for patients who experience dental anxiety or require additional relaxation during the surgery.
Placement of Titanium Implant Posts into the Jawbone
Once the surgical site is adequately numb, the dentist makes an incision in the gum tissue to expose the underlying jawbone. Using specialized surgical instruments, they create small channels or sockets in the jawbone to accommodate the titanium implant posts. These implant posts serve as artificial tooth roots and provide a stable foundation for the dental prosthetic that will be attached later.
Closure of the Surgical Site with Sutures
After the implant posts are securely placed in the jawbone, the dentist carefully closes the surgical site with sutures to promote proper healing and minimize the risk of infection. Depending on the complexity of the surgery and the patient’s oral health status, the dentist may use different suturing techniques to achieve optimal wound closure. The sutures remain in place for a specified period, allowing the surgical site to heal properly and the implant posts to integrate with the surrounding bone tissue.
Overall, dental implant surgery is a precise and meticulously performed procedure that requires skill, expertise, and attention to detail. By following established surgical protocols and utilizing advanced techniques and technologies, dental professionals can ensure the success and longevity of dental implant treatment for their patients. Patients can expect improved oral function, enhanced aesthetics, and restored confidence in their smile following successful dental implant surgery.
Healing and Osseointegration
Healing Process and Osseointegration
After dental implant surgery, the body initiates a natural healing process that is crucial for the success of the treatment. During this period, the gums heal, and the jawbone undergoes a process called osseointegration. Osseointegration refers to the formation of a strong and stable bond between the titanium implant post and the surrounding bone tissue. This process typically takes several months to complete, during which the bone gradually grows and fuses with the implant surface, anchoring it securely in place.
Formation of a Strong Bond between the Implant and Jawbone
Osseointegration is a vital aspect of dental implant treatment as it ensures the stability and longevity of the implant restoration. The formation of a strong bond between the implant and jawbone allows the implant to function like a natural tooth root, providing stability and support for the dental prosthetic attached to it. This bond is essential for withstanding the forces of chewing and biting without compromising the integrity of the implant or surrounding bone structure.
Temporary Restoration Options
During the healing and osseointegration phase, patients may require temporary restoration options to maintain oral function and aesthetics. Depending on the individual case and treatment plan, temporary solutions such as removable dentures, dental bridges, or temporary crowns may be provided to replace missing teeth and maintain proper oral function. These temporary restorations are designed to be functional and esthetically pleasing while allowing for optimal healing and osseointegration of the dental implants.
Abutment Placement
Second Surgical Procedure to Place Abutments
Once osseointegration is complete, and the implant has successfully integrated with the jawbone, the next step in the dental implant process is the placement of abutments. Abutments are small connector devices that attach to the implant post and provide a stable foundation for the final restoration, such as a dental crown, bridge, or denture. The abutment placement procedure typically involves a minor surgical procedure where the gum tissue is reopened to expose the implant and attach the abutment securely.
Healing Time Required Before Proceeding to the Final Restoration
After abutment placement, the gums need time to heal and adapt to the presence of the abutments before the final restoration can be attached. The healing period allows the gum tissue to reposition and form a natural contour around the abutments, ensuring optimal esthetics and function of the final dental restoration.
The duration of this healing phase varies depending on individual healing rates and the complexity of the case but generally ranges from a few weeks to a few months. Once the gums have healed adequately, the dentist can proceed with the fabrication and placement of the final restoration, completing the dental implant treatment and restoring the patient’s smile and oral function.
Final Restoration
Restoring Function and Aesthetics
The final restoration phase of dental implant treatment involves the placement of the permanent dental prosthetic onto the implant abutments. This prosthetic is custom-designed to match the shape, size, and color of the patient’s natural teeth, ensuring a seamless blend with the rest of the smile. The goal of the final restoration is to restore both function and aesthetics, allowing the patient to chew, speak, and smile with confidence.
Types of Final Restorations
Several types of final restorations can be used in dental implant treatment, depending on the patient’s specific needs and preferences. These may include single-tooth crowns, implant-supported bridges, or implant-supported dentures. Each restoration is carefully crafted to provide optimal comfort, stability, and durability while restoring the patient’s ability to bite and chew effectively.
Process of Placement
The process of placing the final restoration typically begins with the removal of any temporary prosthetics that may have been used during the healing phase. The dentist will then attach the permanent restoration to the implant abutments using dental cement or screws, ensuring a secure fit. Once in place, the restoration is checked for proper occlusion (bite) and adjusted as necessary to ensure optimal function and comfort.
Benefits of Final Restoration
The final restoration completes the dental implant treatment process, providing patients with numerous benefits. These include improved chewing ability, enhanced speech clarity, and restored facial aesthetics. Additionally, the final restoration helps to prevent bone loss in the jaw and preserve the surrounding natural teeth by distributing chewing forces evenly across the dental arch.
Post-Treatment Care
Importance of Post-Treatment Care
Post-treatment care is essential for ensuring the long-term success and stability of dental implants. Following dental implant placement and the placement of the final restoration, patients must adhere to a strict oral hygiene routine and attend regular dental check-ups to maintain the health of their implants and surrounding tissues.
Oral Hygiene Practices
Proper oral hygiene practices are crucial for preventing complications such as peri-implantitis (inflammation of the tissues surrounding the implant) and implant failure. Patients should brush their teeth at least twice a day using a soft-bristled toothbrush and fluoride toothpaste. Interdental cleaning with floss or interdental brushes is necessary to remove plaque and debris from between the teeth and around the implants.
Regular Dental Check-ups
Regular dental check-ups are essential for monitoring the health of dental implants and detecting any issues early on. During these appointments, the dentist will examine the implants, surrounding tissues, and prosthetic restorations for signs of inflammation, infection, or other complications. Any necessary adjustments or interventions can be made promptly to ensure the continued success of the dental implant treatment.
Conclusion
Dental implants offer a revolutionary solution for replacing missing teeth and restoring oral health and function. From the initial consultation to the final restoration, the process of dental implant treatment involves several crucial steps, each playing a vital role in the success of the procedure. Understanding these steps and the factors that influence treatment outcomes is essential for patients considering dental implant therapy. By choosing a qualified and experienced dental implant provider and maintaining good oral hygiene habits, patients can enjoy the benefits of dental implants for many years to come.
FAQs
Is dental implant surgery painful?
While dental implant surgery is performed under local anesthesia, patients may experience some discomfort during the procedure. However, most patients report minimal pain and discomfort, which can be managed with over-the-counter pain medications.
How long does it take to complete dental implant treatment?
The duration of dental implant treatment varies depending on individual factors such as the number of implants, the need for additional procedures (such as bone grafting), and healing time. In general, the entire process can take several months to complete.
Are dental implants suitable for everyone?
While dental implants are a highly effective tooth replacement option for many patients, not everyone is a suitable candidate. Factors such as overall health, oral hygiene habits, and the presence of sufficient jawbone are taken into consideration when determining candidacy for dental implant treatment.